Workshop on how to understand the glycocalyx (WS2)
Basic science overview; the Michel - Weinbaum glycocalyx model and the extravascular circulation of albumin and fluid – Tom Woodcock
Notes/Discussions
What happens after an infusion of a hyper-oncotic fluid? The glycocalyx shrinks, releasing plasma volume into the free circulating volume, giving the impression of an increase in vascular volume. If this theory is true, then hyper-oncotic fluids do not draw fluid in from the interstitial space.
Starling’s forces don’t work. Capillaries, in general, cannot reabsorb fluid. A few select capillaries can: gut and renal capillaries for example.
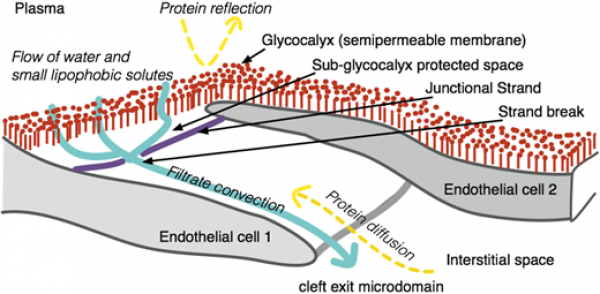
Inflammed capillaries become leaky due to the formation of gaps. Initially these gaps are covered by a layer continuous with the endothelium and has a high reflective coefficient to albumen. What was thought to be small pores, is, in this model, actually a large pore with a selective glycocalyx cover.
Glycocalyx is rooted within the cell cytoplasm, crossing the cell membrane and expressing numerous Glyco-proteins within vessel.
The trans-glycocalyx oncotic pressure gradient is high. The reflective coefficient of the glycocalyx on one side and the flow of water on the other side keep proteins out of the sub-glycocalyx area. This is contra to Starling’s theory.
Starling was dead for quarter of a century before anyone published a ‘Starling Equation’!
Trans capillary escape of albumen is about 5% per hour. In cancer, sepsis and surgery this is 15% (3x higher). How does a cancer patient without shock manage this and yet a septic / post surgical patient becomes oedematous? There is much we don’t understand. It is a function of solvent flux + true diffusion.
Resistance to flow
- junction strands
- Glycocalyx
- Something else!
Interstitial fluid flow is about 8l/day. Thus the entire circulation exits the plasma every 9 hours (possibly every 3 hours in septic patients).
Questions and answers – Tom Woodcock; Can Ince; Bernard van den Berg
Is there any relevance to paediatrics? Nope. This is all animal based and theoretical.
Fluids, glycocalyx and the vascular barrier – Can Ince
Notes/Discussions
The vascular pores and glycocalyx are heterogeneous throughout the vasculature. Different microcirculations regulate flow in different ways.
Cytocam-IDF uses green light to image red blood cells flowing through microvasculature. Video demonstrate giving fluid on its own will increase flow through functional microvascular whilst static and congested capillaries get worse due to interstitial oedema.
Sepsis destroys auto regulation and glycocalyx. Fluid infusions will propagate this and worsen the situation. Reactive oxygen species also increase permeability. Administration of anti-oxidants reduce the destruction of the glycocalyx e.g. Vit C!
Dehydration —> Crystalloids
Hypovolaemia —> Colloids (better than balanced crystalloids and that’s better than normal saline)
Colloids restore MAP and lactate with less volume than crystalloids, but vascular barrier remains unchanged despite choice of fluid.
Summary/Key points
The glycocalyx is not a key component of the vascular barrier.
Protection of vascular function is achieved by anti-inflammatory and anti-oxidant drugs and limitation of fluids.
References
- Where’s the leak in vascular barriers. Kottle SHOCK 2016
- Fluid resuscitation should respect the endothelial glycocalyx Guidet Critical Care 2014; 18:707
- Sepsis and endothelial permeability. Slutsky NEJM
Plasma volume, tissue oedema and the steady-state Starling Principle – Tom Woodcock
Notes/Discussions
Resuscitate with colloid —> patient becomes anaemic
Resuscitate with crystalloid —> patient does not become anaemic
References
Plasma volume, tissue oedema, and the steady-state Starling principle